Welcome progress in Scotland and Wales
It is both a pleasure and a relief to note that the situation regarding pre-exposure prophylaxis (PrEP) in the UK is finally moving forward, most notably in Scotland where a decision was made to make PrEP available to those at the highest risk in July this year. Since then, out of an estimated eligible population of almost two thousand, more than 400 PrEP users have so far commenced NHS funded PrEP. Quite an achievement. Both clinicians and leaders from HIV Scotland have really pushed for change, and continue to do so. Go Scotland!!!


PrEP has been made increasingly available on the NHS, but more still needs to be done
Meanwhile, the Welsh Government and Public Health Wales has also commenced its nationwide PrEP trial; ‘PrEPARED in Wales’. As of October 2017, 6 genitourinary medicine (GUM) clinics in Wales were recruiting to the trial and in contrast with the situation in England, there is no cap on participant numbers. Further details on the trial can be found here www.friskywales.org/wales-prep-project
Where are we with the PrEP IMPACT Trial in England?
The IMPACT Trial in England, a collaboration between NHS England and Public Health England, has very excitingly now enrolled its first patients. St Stephen’s AIDS Trust is providing trial management and a number of community organisations continue to provide input via the Community Advisory Board. IMPACT will provide generic PrEP to 10,000 people, mainly men who have sex with men, with 1,000 places ring-fenced for other communities, such as women and trans people. These places are anticipated to fill up quickly.
The trial, being run from level 3 Genitourinary Medicine (GUM) services, has started in London, Brighton, Sheffield, Nottingham, Liverpool, Manchester, Leicester, Cambridge, Kings Lynn, Bury St Edmunds, Darlington, Durham, Kendal, Carlisle, Workington and Barrow in Furness!! Further roll-out is continuing. The trial enrolled just short of 1,500 people in the first month.
Although many individuals and organisations have been working hard to get the trial started, implementation within more than 200 diverse GUM clinics across England is proving a challenge, as I’m sure many of you are aware. Furthermore, a number of questions regarding implementation remain unanswered, particularly around how best to reach women, and how to capture data appropriately for trans and non-binary people. Other challenges reflect the fragmentation of our specialty, as some GUM services now exist outside the NHS and may not have an associated Research & Development department.
I wonder, is this the largest EVER clinical trial in terms of the sheer number of collaborating centres involved.…? There is still the hope though that NHS England will have an epiphany and realise that full NHS provision is ultimately the answer…. especially as generics are being rolled out in Scotland and elsewhere in Europe. More information on IMPACT can be found HERE
Ensuring that all parts of the community remain informed
With the increased momentum we are now witnessing around IMPACT, it has been particularly encouraging to see a greater emphasis being placed upon ensuring that all parts of the community are as informed as possible. Notably, community organisations have been the main driver behind this, as they have with much of the PrEP education to date.
Before clinics start enrolling PrEPster has a very useful webpage to help guide potential participants: http://prepster.info/impact/5things/


5 things you need to know about joining the PrEP IMPACT Trial from Prepster
Meanwhile the i-Base PrEP Guide, which we all know and (I hope) love, has had an overhaul as well. It reflects the current UK situation with regards to PrEP access, and has new sections on women, trans and non-binary people. It is available online here http://i-base.info/guides/prep and will shortly be available in print. If video information is preferable, I Want PrEP Now have developed some excellent short video clips here https://www.iwantprepnow.co.uk/video-clips
Recognising that much of the conversation around PrEP in the UK has so far focused upon MSM, the Sophia Forum is developing a new website specifically for women and PrEP. It can be found here https://womenandprep.org.uk. CliniQ have developed new literature specifically for trans and non-binary people wanting to use PrEP.
The need to improve PrEP awareness, knowledge, literacy and access in more diverse populations, including BAME (black, Asian and minority ethnic), is as strong and important as ever. However, it’s great to see the first publicly funded HIV Prevention campaign to include PrEP by DoItLondon come to fruition. It includes lots of useful and accessible information on PrEP. It’s perhaps not quite as evocative as my favourite campaign, #PrEP4Love, but it’s definitely a very welcome start ;)
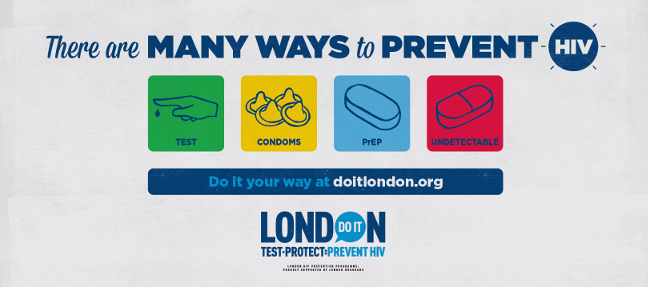
You may have spotted these Do It London posters across the capital
What impact is this likely to have on HIV transmission?
Figures from London sexual health clinic 56 Dean Street published in August ‘17 reported a 40% drop in new HIV infections during the first 6 months of 2017. Furthermore, they estimate a likely 233 new HIV infections to be diagnosed at their site by the end of 2017, down from 679 in 2015 and 393 in 2016. I would like to think that these significant reductions in new HIV diagnoses are in part due to gay men taking responsibility for their own sexual health, and choosing to access generic PrEP, as well as accessing sexual health services. In my mind, there is no doubt that alongside earlier initiation of treatment as prevention, this has played a large role in this truly incredible turnaround. What it definitely does show is that combination HIV prevention works, and that focusing on the specific needs of a community in an innovative, supportive way can pay dividends.
There is increasing data from clinical trials such as the open label extension of Ipergay, worldwide demonstration projects and PrEP roll-outs that show PrEP to be outstandingly effective when taken as directed. It’s also worth bearing in mind that there are still only two reported cases of confirmed HIV transmission for people who were on adequate doses of PrEP and this was due to drug resistant virus. A third case of wildtype HIV reported in an MSM with multiple condomless anal sex episodes and concurrent infection with LGV, may have been aborted if PrEP had been continued. All this goes to show that PrEP really is a game-changer and a quite remarkable HIV prevention tool.
The long-awaited BHIVA/BASHH guideline on HIV Pre-Exposure Prophylaxis will be published shortly - following a recent public consultation - and will provide much more in the way of evidence-based advice on how to make the most of PrEP. Keep your eyes peeled on the BASHH website and Twitter feed (@BASHH_UK) for further details!
And finally, for those who haven’t seen it already, a question for you: What’s the best drug to have sex on? Answer: PrEP! via (@faggotron_). Love it!!
Special thanks to Dr Will Nutland for reviewing this blog and providing permission for use of the ‘Prepster’ image and to Paul Steinberg for providing permission for use of the ‘Do It London’ image.